Károly Vörös1, Márton Balogh1, Christin Kleinsorgen2, Ferenc Manczur1, Ingo Nolte3
Department and Clinic Internal Medicine, University of Veterinary Medicine, István u. 2., 1078 Budapest, Hungary1
E-Learning Consultant of the Veterinary University of Hannover, Foundation, Bünteweg 2; D-30559 Hanover, Germany2
Small Animal Clinic of the Veterinary University of Hannover, Foundation, Bünteweg 9, D-30559 Hanover, Germany3
General information to the digitalized phonocardiograms
Digitalized phonocardiograms (DPCG-s) of this collection were recorded by a Welch-Allyn Welch Allyn Meditron System as described by Vörös et al. 2011. The illustrated digital phonocardiogram (DPCG) diagrams contain simultaneous Einthoven II ECG recordings and the mechanical events (digital phonocardiograms) of the cardiac cycles. It is suggested to first listen to the audio recordings “blindly”. These audio files were converted by Audacity® (https://www.audacityteam.org) from the original, special Welch Allyn Meditron .wav files (which contain both the simultaneous ECG and sound channels, however being playable only with the Welch Allyn Meditron software). After listening to the audio sound files, the interested user is suggested to listen and observe the DPCG video recordings which can help to memorize the characteristic auscultatory features of the different arrhythmias by watching simultaneously the DPCGs including their synchronized ECG recordings, as a cognitive process. DPCGs were converted from the original Welch Allyn Meditron .wav files with the CamStudioTm (www.camstudio.org) from the original Welch Allyn Meditron DPCG video recordings. The audio and video illustrations are labelled with the numbers of the relevant paragraphs of this document, added with numbers of the recording within the text e.g., in paragraph one: normal cardiac rhythm and electrocardiogram (Nr. 1.1. audio and video). Some recordings also contain cardiac murmurs together with the demonstrated arrhythmia. A detailed description and examples of canine cardiac murmurs can be found in the relevant part of this heart sound library.
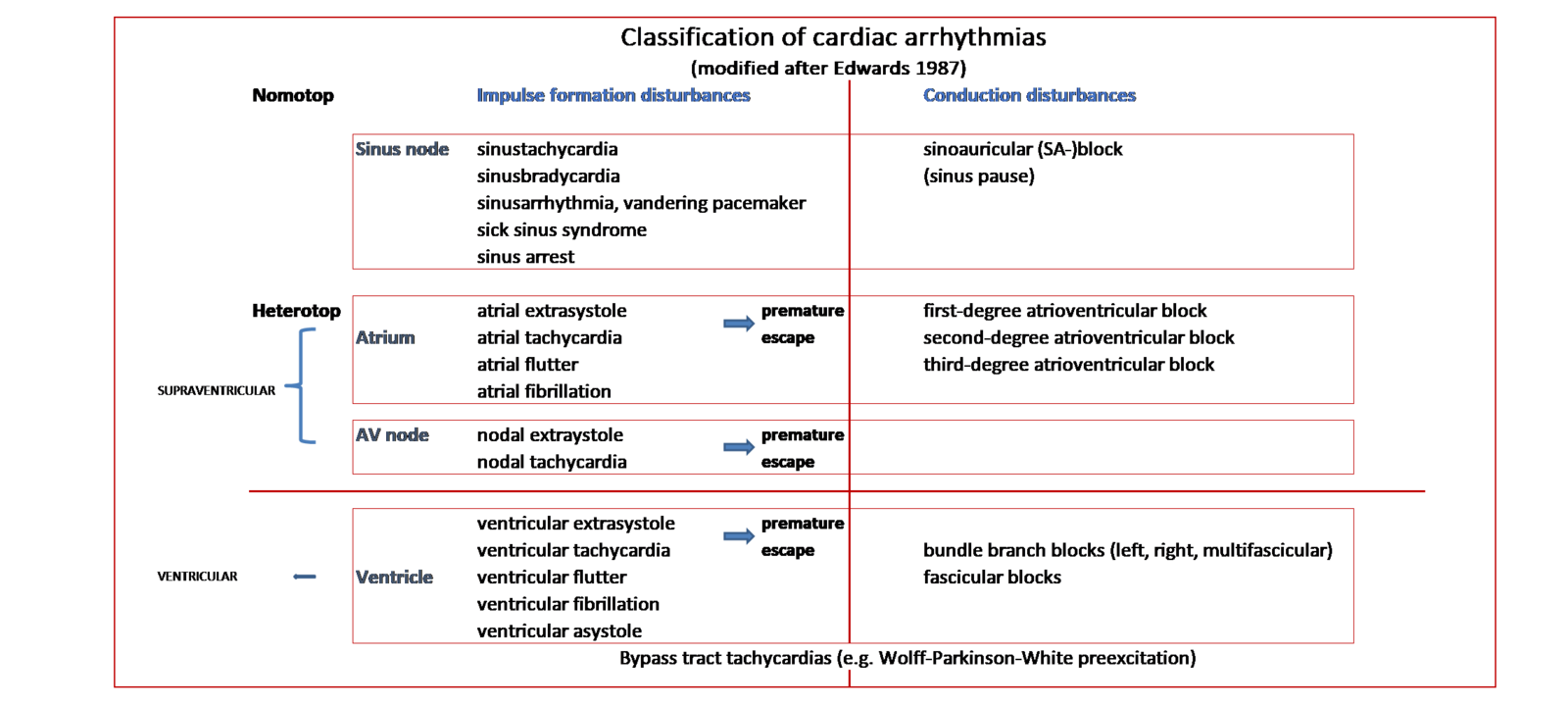
Those arrhythmias which are not illustrated with DPCGs are marked with black within the text (without audio and video files) e.g., in paragraph six: sinus arrest (Nr. 6.1.). However, the collection of the DPCG-s is upgraded regularly. The classification of cardiac arrhythmias is demonstrated on the Figure.
Classification of cardiac arrythmias
Description of cardiac arrhythmias
- The normal cardiac rhythm and electrocardiogram (Nr. 1.1. audio and video) are characterized by a normal heart rate, regular rhythm, and physiologic ECG. The term cardiac arrhythmia means (all) abnormalities of the impulse formation and conduction system of the heart, regulated by sympathetic and parasympathetic neurohormonal stimuli. Although the meaning of the Latin word arrhythmia is “no rhythm”, it is used for all irregularities, even for those which are (more or less) coinciding with a regular cardiac rhythm (e.g., sinus bradycardia and sinus tachycardia). As such, the technical term dysrhythmia would be a better (i.e., more precise) expression. Nevertheless, “arrhythmia” is used generally, both in the human and veterinary terminology. Cardiac arrhythmias can be of intracardiac and extracardiac origin, and might be benign or pathological. Idiopathic or primary arrhythmias are related to the direct disturbances of the intracardiac impulse formation and/or connection system (e.g., ion channel mutations, fibrosis, amyloidosis etc.). Secondary arrhythmias can be the results of cardiac remodeling during structural heart diseases (e.g., myxomatous mitral valve disease) or related to extracardiac disorders (e.g., pancreatitis, gastric volvulus, hyperkalaemia etc.).
Types and electrophysiological classification of cardiac arrhythmias (See on Figure as well)
Impulse formation disorders
Nomotop impulse formation disorders
These arrhythmias originate from the physiological center of the impulse formation i.e., from the sinus node.
2. Sinus tachycardia (Nr. 2.1. audio and video) is a regular, accelerated rhythm with a normal electrocardiogram (ECG). On these recordings, a systolic cardiac murmur of grade 5/6 can also be heard and seen which was caused by mitral insufficiency.
The lower limits of sinus tachycardia:
in dogs >160-180 /bpm, in cats: >180-220/bpm (depending on the behavior of the animal i.e., how calm or excited is the patient)
3. Sinus bradycardia (Nr. 3.1.1. audio and video) is a regular, slower than physiologic rhythm, with a normal ECG. In dogs, sinus arrhythmia (see below) is often observed, whilst regular sinus bradycardia is rare. On Nr. 3.1.2. audio and video recordings, bradycardia with isolated ventricular extrasystole (VES) being obvious at the 8th sec on the DPCG can be observed. (Definition of VES see below at heterotop impulse formation disorders.)
The upper limits of sinus bradycardia:
dogs: <60 /min
cats: <140/min
4. Physiologic sinus arrhythmia, also named physiologic respiratory arrhythmia (Nr. 4.1. audio and video) is due to expressed parasympathetic vagus effect during expiration. It is characterized by a lover cardiac rhythm regarding expiration compared to inspiration. On the ECG, the R-R intervals are gradually prolonged and then shortened related to the expiratory and inspiratory phases of respiration. The phenomenon “wandering pacemaker” can sometimes also be recognized on the ECG represented by different heights (voltages) and shapes of the P waves. The shape of the P waves is taller during inspiration and smaller during expiration.
5. Sick sinus syndrome (5.1.) is a disease of the sinus (sinoatrial) node and that of the atria. It consists of sinus bradycardia, sinus arrest together with escape beats (late extrasystoles) or even escape rhythms and/or supraventricular tachycardia. Some textbooks classify this disorder as a combined impulse formation and conduction disturbance.
6. Sinus arrest (6.1.) means that the R-R interval is longer than that of two normal sinus beats.
Heterotop impulse formation disorders
7. Extrasystoles are characterized by an irregular appearance of the relevant cardiac compex on the ECG curve depending on their origin. The myocardial localization of an extrasystole can be determined by the presence or lack of the P wave and its relationship to the QRS complex as well as by the shape of the QRS. A heterotop impulse formation disorder can originate from the atria i.e., atrial ES (7.1. audio and video). On this DPCG, an isolated premature atrial extrasystole (AES) without a P wave can be seen and heard at the 1st sec (It is the 4th cardiac complex). On these recordings, a systolic cardiac murmur of grade 4/6 can also be heard and seen which was caused by mitral insufficiency. Extrasystoles can also arise from the Aschoff-Tawara (atrioventricular) node (7.2.) or from the ventricles (7.3. audio and video). On this DPCG, isolated premature ventricular extrasystoles (VES) of bizarre shape can be seen and heard at the 2nd, 6th, and 15th sec. An extrasystole can be active (early, premature beat), represented by an abnormal cardiac complex arising on the ECG as the consecutive sinus beat would be expected (7.4. audio and video). On these recordings, two VES with different, bizarre ventricular complexes can be seen and heard at the 7th and 8th sec on the DPCG. A premature atrial extrasystole (AES) similar to a normal ventricular complex but without a P wave is also present at the 11th sec. As such, these three ES are of different forms which represent a multifocal origin from the cardiac musculature.
A “late extrasystole” named escape beat (Nr. 7.5.) is represented by an abnormal cardiac complex appearing later on the ECG where the consecutive sinus beat would be expected. Ventricular escape beats act to prevent cardiac arrest. They are common during impulse conduction disorders if they arise with long pauses (see the relevant chapter below).
8. Supraventricular tachycardia means a sustained or temporary (paroxysmal) run of premature, supraventricular extrasystoles (i.e., more than 3 consecutive abnormal beats). They can be of atrial or nodal origin (Nr. 8.1.).
9. Atrial fibrillation (AF) (Nr. 9.1. audio and video) is due to abnormal impulse formation originating from the atria. The AF is characterized by a completely abnormal (chaotic), usually fast rhythm, lack of P waves, presence of f waves (not always visible) and by more or less normal QRS complexes with irregular R-R intervals. On these recordings, a cardiac murmur of grade 3/6 can also be heard and seen which was caused by mitral insufficiency. Atrial fibrillation and isolated VES can also occur (Nr. 9.1.2. audio and video). On these recordings a premature ventricular complex can be seen and heard on the DPCG at the10th sec. At the 4th sec, a suspected ES can also be heard on the DPCG without a cardiac complex on the ECG. This might be because this complex can be perpendicular to the single, applied ECG lead, not producing electrical signals on these recordings. Multichannel ECG is needed in these cases to identify these ES. (See further examples below).
10. Atrial tachycardia (Nr. 10.1. audio and video) is a type of SVT, and defined as a focal (often very fast) tachycardia originating from the atrial muscle. Note that on the ECG, the P-waves are often not visible (can be buried within the ST-segment or T-wave of the previous cycle).
11. Atrial flutter (Nr. 11.1.) is similar to atrial fibrillation; however, the F waves are larger than the f waves and the R-R intervals are more regular.
12. Ventricular extrasystoles (VES) can be isolated i.e., single (12.1. audio and video). On these recordings, a premature ventricular complex can be seen and heard on the DPCG at the 8 th sec. At the 3rd sec, a suspected ES can also be heard on the DPCG without a cardiac complex on the ECG (see explanation above). VES can also occur in pairs named couplet (12.2.) or in triplets (12.2.1). In bigeminia (12.3.) every regular sinus beat is followed by a premature beat. During trigeminia (12.4.) two sinus beats are followed by a premature beat. Multifocal extrasystoles demonstrated on 7.4. (audio and video) originate from different parts of the ventricles or from the atria and have different morphology of the QRS complexes. Sometimes an extrasystole can’t be seen on the ECG if only one ECG lead is used. However, it might be heard during auscultation and can be seen on the DPCG as already demonstrated and explained above. On the recordings 12.1. (audio and video) a premature VES with bizarre cardiac complex can be seen and heard at the 8th sec. A suspected ES is present at the 3rd and 9th sec which can’t be seen on the ECG but are visible and audible on the DPCG. 12.5. The idioventricular rhythm is very similar to ventricular tachycardia except the ventricular rate is less than 60 beats/minute in dogs. This occurs in a run of ventricular escape beats. Idioventricular rhythm is frequently referred to as “slow ventricular tachycardia”. When the ventricular rate is between 60 and 100 beat/minute, it is called an accelerated idioventricular rhythm. This can happen after myocardial trauma e.g., during car accidents. On 12.6. (audio and video) a premature ES can be remarkably heard and seen on the DPCG at the 6th sec but is is not present on the ECG. Multichannel ECG (not shown) revelaed premature VES. Sinus arrhythmia with different RR intervals and with normal sinus beats as well as a systolic grade 5/6 murmur caused by mitral insufficiency is also present.
13. Ventricular tachycardia (VT) is characterized by a run of four or more premature ventricular beats. P waves are not present during the runs of ventricular beats (which are often faster than the phase of the sinus beats in the paroxysmal form). The R-R intervals are more or less regular during VT. It can be sustained (13.1.) or non-sustained (paroxysmal). On (13.2. audio and video) demonstrating paroxysmal ventricular tachycardia (PVT), a run of bizarre ventricular complexes can be seen followed by fast, regular sinus beats. As the frequency of PVT and sinus beats are nearly the same, it is not to distinguish them by simply listening to the recordings, although they are obvious on the ECG. On 13.3. (audio and video) two types of VES runs can be recognized with different ECG shapes and frequency as well as sound intensity, between regular but fast sinus beats.
14. Ventricular flutter, ventricular fibrillation, and ventricular asystole. These severe electrocardiographic disturbances are signs of the direct danger of cardiopulmonary arrest (CPA) requesting immediate cardiopulmonary resuscitation (CPR). During ventricular flutter (14.1.) there are regular ventricular activities, but the QRS waves and the T waves cannot be distinguished. In ventricular fibrillation (14.2.) the electrical activity of the ventricles is characterized by chaotic baseline undulations with irregular ECG waveforms. The complete or final ventricular asystole (ventricular arrest, cardiac arrest) (14.3.) means that the electrical activity of the ventricles is confined to wide and bizarre baseline undulations or extrasystole-like complexes with long periods of straight baseline. Temporary ventricular arrest might occur during sinoatrial (sinus) arrest.
Conduction disturbances (disorders)
Nomotop conduction disorders
15. A sinoauricular (sinoatrial) block (15.1.) is characterized by a longer pause between two sinus beats as the consecutive sinus beat (R-R interval) would be expected. In this conduction disorder, the sinus node (sinoatrial node) discharges normal impulses, but they are not conducted to the atria. The form of the ECG is normal during all beats. The R-R- interval during the block is equal to that of two normal sinus beats. The sinoatrial block and the sinus arrest (see above) have the same clinical features and it has no importance to differentiate them in this respect.
Heterotop impulse conduction disorders
16. The first-degree atrioventricular block (Nr. 16.1.) is represented by a prolonged PR (or PQ) interval. Otherwise the rhythm and the ECG configuration are normal, as all impulses are conducted to the ventricles (although delayed).
17. The second-degree atrioventricular (AV) block is characterized by isolated P waves without consecutive QRS complexes when the impulse is not conducted from the atria to the ventricles. They can be isolated (17.1. audio and video) as heard and seen as the atrial sounds/contractions at the 1st, 2nd, 4th, and 6th sec., etc. or might occur in runs (17.2.) followed by escape beat(s). However, the atrial sounds might be difficult to recognize during auscultation due to their low intensity, especially in small dogs. In the Mobitz 1 (Wenkebach phenomenon) type second-degree AV block (17.3.) the PR interval becomes progressively longer, until a QRS complex is dropped. The Mobitz 2 type second-degree AV block (Nr. 17.4.) is characterized by constant PR intervals (before the dropped beat). A high-grade second-degree AV block (Nr. 17.5.) means that the P:QRS ratio is 3:1 or higher. The high-grade second-degree AV block is similar to the third-degree AV block. In this type of AV block however, there is still some relationship between the P waves and the QRS complexes which helps to differentiate it from the third-degree AV block.
18. The third-degree AV block (Nr. 18.1. audio and video) is the most severe form of the AV blocks when all atrial impulses are blocked at the AV node. Therefore, the atria and the ventricles work independently, and both have their own rate. The QRS-complexes are escape beats originating from the His-bundle or from the ventricles with a much lower rate in comparison to that of the atria. As such, there is no association between the P waves and the ventricular complexes. This phenomenon is also called atrioventricular dissociation. On the present recordings, the P waves are not clearly seen on the ECG, but the atrial contractions can be heard, and they are well seen on the DPCG e.g., at the 1st, 3rd, and 6th sec etc. The ventricular sounds are slower and louder whilst the atrial sounds are faster and stiller. As such, the auscultatory finding of the third-degree AV block is characterized and can be mimicked with the onomatopoetic sounds “Boom! pit, pit, pit, boom! Pit, pit, pit, boom!”, Nevertheless, the atrial sounds might be difficult to hear during auscultation due to their low intensity, especially in small dogs. Therefore, this characteristic sound combination is not easy to recognize, and usually the term of irregular auscultatory finding can be applied.
19. Bundle branch (Tawara branch) blocks are characterized by disruption of the impulse conduction through a bundle of His. Depending on their location, they can manifest in the following forms: Left anterior fascicular block, left bundle branch block, multifascicular block, and right bundle branch block. None of them coincide with an abnormal auscultatory finding (Nr. 19.1.).
Impulse formation and impulse conduction (combined) disorders
20. Bypass tract tachycardias (also named ventricular preexcitations) are due to one or several accessory pathways (e.g., Paladino-Kent branch) that bypass the normal atrioventricular conduction pathway. One example is the Wolff-Parkinson preexcitation (Nr. 20.1.). The heart rate during the tachycardia is usually very high (>300/min) and negative P-waves are following the QRS-complexes (buried in the QRS-complex or in the ST-segment). At normal heart rates “Delta waves” (preexcitation) may be visible on the QRS-complex whilst the PQ(PR) intervals can be abnormally short.
Literature
Balogh, M., Koch, F., Siver, L., Krima, A., Vörös, K. (2021): Digital phonocardiography of cardiac arrhythmias in dogs - Preliminary experiences. Acta Vet. Hung., 69. 116-124.
Balogh,, M., Rishniw,, M., Vörös,, K (2022).: Remote teaching of canine cardiac auscultation using digital phonocardiograms. J., Vet. Med. Educ., 2022. https://doi.org/10.3138/jvme-2021-0097 pp 1-6.
Balogh, M., Vörös, K. (2022): The role of cardiac auscultation and digital phonocardiography in the diagnosis and education of canine heart diseases. Literature review and own experiences. (In Hungarian). Magy. Állatorvosok Lapja, 144. 341-350.
Blass, K. A., Schober, K. E., Bonagura, J. D., Scansen, B. A., Visser, L. C., Lu, J., Smith, D.N., Ward, J.L. (2013): Clinical evaluation of the 3M Littmann Electronic Stethoscope Model 3200 in 150 cats. J. Feline Med. Surg. 15. 893-900.
Edwards, N.J. (1987): Bolton’s handbook of canine and feline electrocardiography. 2nd ed., W.B. Saunders Co., Philadelphia.
Ettinger, S.J., Feldman, E.C., Cote, E. (2017): Textbook of veterinary internal medicine. Diseases of the dog and cat. Expert consult, 8th ed., Saunders, St. Luis, 2017.
Germanakis, I., Dittrich, S., Perakaki, R. and Kalmanti, M. (2008): Digital phonocardiography as a screening tool for heart disease in childhood. Acta Pediatr. 97. 470-473.
Germanakis, I.; Kalmanti, M. (2009): Paediatric cardiac auscultation teaching based on digital phonocardiography. Med. Educ. 43. 489. doi: 10.1111/j.1365-2923.2009.03343.x.
Koch, F: Digital sound processing in the diagnosis and teaching of canine cardiac arrhythmias. (in Hungarian). Diploma thesis, University of Veterinary Medicine, Budapest, Hungary, 2017.
Killich, M. (2019): Kleintierkardiologie. Diagnose und Therapie von Herzerkrankungen bei Hund, Katze und Heimtieren. (in German). Georg Thieme Verlag, Stuttgart, New York.
Kvart, C; Häggström, J. (2002): Cardiac auscultation and phonocardiography in dogs, horses, and cats. Published by Clarence Kvart, Uppsala.
Naylor, J., Yadernuk, L.M, Pharr, J.W., Ashburner, J.S. (2001): An assessment of the ability of diplomates, practitioners, and students to describe and interpret recordings of heart murmurs and arrhythmia. J. Vet. Intern. Med., 15. 507–515.
Nelson, R. W. and Couto, C. G. (eds.): Small animal Internal medicine. 5th ed. Mosby, St. Luis.
Rijnberk, A.; van Sluijs, F.J. (2009): Medical history and physical examination in companion animals. 2nd ed., Saunders, Elsevier, Edinburgh.
Sisson, D. and Ettinger, S.J.: The physical examination. In: Fox, P. R., Moïse, N. S. and Sisson, D. (eds) Textbook of Canine and Feline Cardiology. Principles and Clinical Practice. 1999. 2nd edition. W. B. Saunders, Philadelphia. pp. 46–64.
Smith, F.W.K., Tilley, L.P, Oyama, M.A., Sleeper, M.M. (2015): Manual of canine and feline cardiology. 5th ed. Elsevier, St. Luis.
Szilvási, V., Vörös, K., Manczur, F., Reiczigel,J., Novák, I., Máthé, Á., Fekete,, D. (2013): Comparison of traditional and sensor-based electronic stethoscopes in Beagle dogs. Acta Vet. Hung., 61. 19-29.
Tobias, R., Skrodzki, M., Schneider, M. (2008): Kleintierkardiologie kompakt. (in German) Schlütersche Verlag GmbH, Hannover.
Tilley, L.P. (1992): Essentials of Canine and Feline Electrocardiography: Interpretation and Treatment. 3rd ed. Lea & Febiger, Philadelphia.
Vörös, K.: The role of physical examination in the diagnosis of cardiac diseases (in Hungarian.) Kisállatpraxis, 2010. 11. (1.) 2-10.
Vörös, K., Nolte, I., Hungerbühler, S., Reiczigel, J., Ehlers, J.P., Tater G., Mischke R., Zimmering, T., Schneider, M. (2011): Sound recording and digital phonocardiography of cardiac murmurs in dogs by using a sensor-based electronic stethoscope. Acta Vet. Hung. 59, 23-35.
Ware, W. A.: Cardiovascular disease in small animal medicine. Manson Publishing, London, 2007.




